GUEST BLOGGER: Kathryn Biel.
Marcia submitted this clinical question:
Any ideas on how to improve gait and balance in an 11 year old with dystonia? Backwards gait is OK but forward stepping is very ataxic and asymmetry increases with increased speed. Nothing seems to help consistently. HELP!!
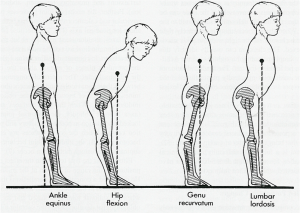
Dystonia, for me, is one of the most difficult tone issues to work with, around, through. I always feel sort of lost and like I’m grasping at straws. Here’s where I would start: muscle length and muscle strength. What’s short and tight? What’s long and weak? I would guess that the flexors are stronger in relation to the extensors, since backward walking is better than forward. Is one side more dominant than the other? Stretch what’s tight, and strengthen what’s weak. This might be a case where, to improve walking, you take a few steps back and just strengthen. Look at the hip extensors and lateral musculature specifically.
Biofeedback and the use of mirrors during treatment can help to give the patient an awareness of his or her movement patterns, which may aid in some postural corrections.
If there is a muscle imbalance due to dystonic spasms in the opposing muscle, modalities could be indicated. This could include NMES to the antagonistic muscle groups (which oppose the dystonic, spasming muscles) to increase muscle strength. Kineseotaping to both inhibit and facilitate may be a valuable tool. Although this child is a little old (for social reasons), compression and strapping garments (like TheraTogs) may also be useful.
Tone management (like Botox injections that would specifically target muscles) may be indicated, and are often prescribed in dystonia. Patient and family education on tone management is important.
Dystonia is a very difficult condition to treat. If you have other ideas or suggestions, please feel free to comment. I’d love to hear about what has been successful for you.
~Kathryn Biel, PT, DPT
]]>

 Kathryn Biel[/caption]
Kathryn Biel[/caption]